In a piece published on June 13, 2018 in The Wire, Anand Grover takes issue with several pieces that I have written regarding the approval of bedaquiline, a new drug meant to treat a certain type of multi drug resistant tuberculosis (MDR). Surprisingly, he doesn’t refer to my sixth piece on the issue, published on Newslaundry, where I discuss the law on clinical trials.
While I’m glad that we are debating this issue, I disagree with Grover on multiple issues.
Cherry picking data on bedaquiline
To briefly recap the facts of this debate – Janssen & Janssen a pharmaceutical company discovered a new drug called bedaquiline. It is one of the first new drugs developed in the last 40 years that shows promise in treating MDR. The government is controlling access to the drug by administering it only through government hospitals – the data collected from these government hospitals is then given to Janssen (both parties signed a data sharing agreement). Like Grover, there are several other activists who are arguing for more patients to be given access to the drug on the grounds that it is the last hope for patients with XDR i.e. extensively drug-resistant tuberculosis. The problem, however, is that the drug has only cleared Phase II trials and is still undergoing Phase III trials which will conclude only in 2021.
This is an important point to note because a lot of drugs that clear Phase II, fail Phase III trials. An industry study revealed that only 55% of drugs clear Phase III trials because these trials are more rigorous since they have more patients and are meant to conclusively establish safety and efficacy of the drug. Since bedaquiline hasn’t completed Phase III trials, the medical community simply lacks the data to conclusively determine the safety and efficacy of the drug. One of the reasons this drug needs more safety data is because the cohort that was administered bedaquiline in the Phase II clinical trials reported a larger number of deaths than the cohort which did not receive the drug. While causation is yet to be proved between the drug and the deaths, there is enough reason to be apprehensive about the safety of the drug since the clinical trials have also reported that a side-effect of bedaquiline is increased Qt prolongation of the heart, which basically means that there were some alterations to the electrical activity of the heart. The Phase II study can be read here.
In countries like the US, which have granted bedaquiline conditional approval (a regulatory pathway that doesn’t exist in Indian law), Janssen is forced to carry a blackbox warning on the packaging of the drug stating the following: “An increased risk of death was seen in the SIRTURO treatment group (9/79, 11.4%) compared to the placebo treatment group (2/81, 2.5%) in one placebo-controlled trial”. The USFDA also requires Janssen to inform patients that the safety and efficacy of the drug is yet to be established. On the other hand, the consent form drawn up by the Indian government for Indian patients being treated at government hospitals is entirely silent about these adverse side-effects. The consent form can be accessed here at page 4 and the patient information booklet is in the preceding pages – neither mention the past history of this drug.
Notwithstanding these serious issues raised by medical practitioners and regulators, activists like Grover describe bedaquiline in glowing terms. Grover justifies his enthusiasm on the grounds that the World Health Organisation (WHO) has recommended the drug. It should be stressed that the WHO guidance is ‘interim’ in nature which means that even the WHO is yet to form a final opinion and will not do so until it has Phase III data. In the case of another new TB drug called delaminid, the WHO revised its interim guidance after the drug disappointed in Phase III clinical trials. So, I would take the interim guidance with a pinch of salt.
Grover also claims that the WHO’s latest assessment shows that 63% of the patients administered bedaquiline were cured. That is not an accurate description of the WHO’s report because bedaquiline was only one of the drugs in a multi-drug treatment i.e. bedaquiline is being prescribed along with other drugs. The same WHO assessment also mentions that 30% of the patients experienced Qt prolongations – meaning that the electrical activity of their heart was being affected as reported in earlier trials. The good news, however, from the same document, is that there were no mortalities in the later trials and hence the WHO decided to downgrade the risk of undesirable effects from large to moderate, which although better, still represents a risk.
The question that flows from above discussion is how did Indian authorities approve this drug when Phase III trials were not complete especially when the drug has known safety issue? The issue of approval is different from the issue of whether the drug could be given to MDR patients in India if it was not first approved by the DCGI but since the latter issue has caused more concern let me tackle that issue first.
Could bedaquiline have been provided to patients in any other manner?
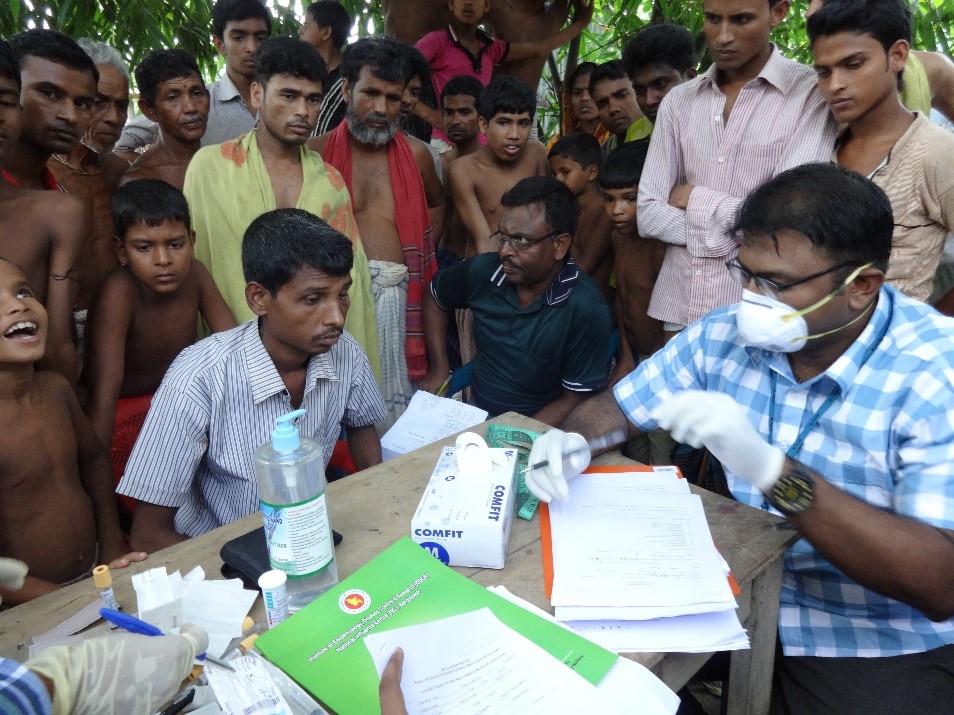
On reading Grover’s piece, one gets the sense that bedaquiline could not have been provided to patients unless the DCGI approved it immediately without waiting for results from Phase III clinical trials that are due in 2021. As I explained in the Newslaundry piece, it was perfectly possible for the government of India to sponsor a clinical trial for all the patients. In the last three years, the government has provided bedaquiline to approximately 1,000 patients through six hospitals – that’s about the size of a large clinical trial. If the government had sponsored the trial and registered the same as per the law it would have been forced to safeguard patient rights.
This would have meant a right to compensation, under Rule 122DAB, in case the drug caused the death of patients or any other injury to them (as of now the bedaquiline consent form at government hospitals forces patients to waive any right to compensation). The entire treatment plan would have been vetted by an ethics committee. Any serious adverse events during the course of the trial would have to be mandatorily reported to the DCGI. The informed consent form would have to meet the requirement of Appendix V to ensure that patients had complete information. These are just some of the safeguards that would have been in place if the treatment was granted through a clinical trial process. Many of these safeguards have been inserted after the HPV scandal – people have lost their lives before these safeguards were inserted into the law.
In my interaction with one of my other critics, she claimed that only Janssen as the patentee and not the government could have sponsored a clinical trial. This is not true – as long as an institution has access to the drug it can seek approval to carry out a clinical trial. There is no requirement under the law for only the patentee to carry out the trial. In the case of bedaquiline, Janssen is anyway donating the drug to the Indian government for free. If the government had access to the drug, it should have nominated a hospital or research agency to sponsor a clinical trial. Instead, we have a scenario where Indian patients are being administered a drug by the government in an unethical manner while activists cheer on the government.

Chemical structure of bedaquiline. Credit: Wikimedia Commons
The regulatory approval granted to bedaquiline
In his piece Grover disputes my interpretation of the law, in particular my assertion that Phase III trials cannot be waived under Rule 122A of the Drugs & Cosmetics Rules, 1945 and that the DCGI could not have approved bedaquiline until Phase III trials are complete. He contradicts my conclusion by saying that “Nowhere do the rules require that data from Phase III clinical trials be available to the DCGI. They only say that relevant “data is [to be] available from other countries.” In plain English, Grover makes the point that as long as “data” is available it is of no consequence whether that data is from a clinical trial or from other sources – to burnish his point he cites data from the WHO to claim that the data was in fact available.
His interpretation of the law is incorrect, as I will explain later, but let’s presume for a moment that he is correct in his interpretation that only data is required and not clinical trials. The problem with the “data” that he quotes is that the DCGI approved bedaquiline on January 14, 2015 while the WHO data that downgraded the risk associated with bedaquiline from “large” to “moderate” is from 2017. In any event, it is obvious from the minutes of the Technical Committee that the government considered only the US and EU approval and not WHO data while deciding to waive clinical trials. Even on this count, the Technical Committee was incorrect in its assessment because bedaquiline got only conditional approval after Phase II trials data in both jurisdictions – Phase III trials were not complete and hence bedaquiline could not get final approval. The Committee also appears to be ignorant of the difference between conditional approval and final approval. Don’t forget that the USFDA made it clear to Janssen that it had to inform patients that the safety and efficacy of the drug was not established since Phase III trial data was pending. How can the Technical Committee depend on such an approval to waive clinical trials for a drug with known safety issues?
Rule 122A read with Schedule Y mandate Phase III clinical trials
Grover also argues that Rule 122A never mentions the phrase “clinical trial” and that it only requires “data” which can come in other forms and not just through clinical trials. Grover has clearly missed the part in Rule 122A that requires all new drug applications to be accompanied by “information and data as required by Appendix I or Appendix IA of Schedule Y, as the case may be.” Schedule Y lists all data that is to be submitted to the DCGI – in particular Clause 1(iv) of Schedule Y, identifies the following as relevant data: “…human clinical pharmacology data as prescribed in Items 5, 6 and 7 of Appendix I”. A reference to Items 5, 6 & 7 of Appendix I indicates that those items reference Phase I, Phase II & Phase III clinical trials as described in Schedule Y which can be accessed here. It is thus clear that data for Phase I, Phase II and Phase III clinical trials is required to be submitted to the DCGI.
I therefore do not understand how Grover is claiming that Rule 122A requires only “data” and not “Phase III clinical trials”.
Can Phase III trials be waived?
The issue now is whether Phase III trials can be waived. Under Indian law, Phase I trials are safety trials meant to establish the toxicity of the drug on healthy volunteers. Phase II is a therapeutic exploratory trial on a small number of patients to understand the efficacy of the drug. If Phase II results are promising the drug moves to Phase III trials which are therapeutic confirmatory drugs that establish the efficacy of the drug on a large number of patients and helps determine the risk/benefit of the drug.
Phase III trials in India are usually split into two parts: clinical trials conducted outside the country and local clinical trials conducted within the country. Schedule Y, states in pertinent part that “For new drugs approved outside India, Phase III studies need to be carried out primarily to generate evidence of efficacy and safety of the drug in Indian patients when used as recommended…”. These are the local clinical trials referred to in Rule 122A.
Thus, even if a drug has been approved in foreign jurisdictions based on clinical trials in those countries, the law requires the drug to be tested on an Indian population to validate the drug in the Indian context. This requirement for local clinical trials however can be waived under the proviso to Rule 122A provided the drug is already approved in foreign countries. The proviso states in relevant part:
“Provided that the requirement of submitting the results of local clinical trials may not be necessary if the drug is of such a nature that the licensing authority may, in public interest decide to grant such permission on the basis of data available from other countries”.
It should be noted that the above proviso does not state “Phase III trials” may be waived – it only states that “local clinical trials” may be waived, which clearly means that the rulemaker was expecting some kind of Phase III trials. Thus, if the drug had approvals from the US or EU based on Phase III data the local clinical trials in India could be waived. But as discussed earlier, the US and EU approvals were conditional since their regulators were still awaiting Phase III data.
Apart from the proviso to Rule 122A, Grover in his latest piece makes a new argument by citing the following provision from Schedule Y to defend the DCGI’s decision:
“For drugs indicated in life-threatening/serious diseases or diseases of special relevance to the Indian health scenario, the toxicological and clinical data requirements may be abbreviated, deferred or omitted, as deemed appropriate by the Licensing Authority.”
He claims that the bedaquiline fits the above criteria and hence he supports the DCGI’s decision to approve the drug sans trials. Open ended provisions like the one above do not give the government a blanket licence to act as it pleases. As Grover will surely admit, all administrative decision making has to be reasonable not capricious or arbitrary. In the case of bedaquiline, when the USFDA and WHO have both flagged the safety concerns, it is rather incredible for Grover to cite the above provision to defend waiving all clinical trials of a drug that demonstrated cardiotoxicity in Phase II trials. What then is the point of clinical trials and drug regulation if the regulator can waive trials of a drug with known safety issues? What of the human rights of the patient?
Now that a former UN Special Rapporteur on the Right to Health has offered the above provision as a get out of jail free card expect more pharmaceutical companies to invoke the provision to seek complete waivers.
This article originally appeared on SpicyIP.
§
Anand Grover responds:
This is in response to Mr. Prashant Reddy’s to my article in The Wire, titled Debate: India’s TB Patients Need Bedaquiline Now, Never Mind the Critics.
Before proceeding further I must make it clear that I don’t believe in making personal attacks or innuendos, which Mr. Reddy has unfortunately resorted to. That only detracts from the serious points he makes. I take what he says very seriously because I respect the points he makes. It is in that spirit that I wrote my initial article and I am penning this rejoinder. Just for the record, if Mr. Reddy is unaware, I argued leading cases on access to medicines, for patients’ rights, including the Novartis cases, the compulsory licensing of Natco against Bayer and the HPV case on which he bases his arguments on compensation.
Mr. Reddy makes three points.
First, the manner in which the government is collecting data for Janssen is in total disregard of ethics and the rights of persons being administered bedaqualine. This is indeed a very serious issue that he has raised and I have already indicated that the government has a lot to answer, which it should.
Second, the data for Bedqualine does not indicate that it is safe; in particular, it has not passed the muster of phase III trials abroad.
Third, in view of the absence of data from Phase III trials, the Drug Controller General of India (DCGI) could not have given marketing approval, though limited through government hospital, to bedaqualine.
Before I go to the points, it is important to point out that the emergent nature of the TB and the multi-drug resistant (MDR) epidemic and the deaths it is causing in our country, which is the context of my argument, is sadly, completely absent in the discourse of Mr. Reddy. The huge number of people dying in India on account of this deadly disease is totally lost on him. Repeatedly, in my work as an activist, which appears to be a pejorative term for Mr. Reddy, and as a lawyer fighting for access to medicines, I have seen how peoples’ lives turn to the better when medicines, which were being denied to them, are made available to them.
In the context of TB, this happened to the girl in Patna, who got bedaqualine, for MDR TB, whose case I fought before the Delhi high court. Today, she is alive, having faced death on account of denial of bedaqualine. I have also seen how people’s lives are destroyed because they cannot access medicines, which could have saved them, primarily because of bureaucratic apathy. I would submit that if one does not take into account the deaths admittedly occurring on account of TB and MDR TB in India, for which bedaqualine provides a ray of hope, which, in my opinion, is a good one, I might also have come to the conclusion that Mr. Reddy does, based only on a textual reading of the law. Then it doesn’t matter what happens to people whether they live or die. We cannot proceed on that basis.
I would now take up the legal point relating to the approval, which is the core of my argument, before the point on safety of Bedaqualine.
To quote Mr. Reddy:
“Grover also argues that Rule 122A never mentions the phrase “clinical trial” and that it only requires “data” which can come in other forms and not just through clinical trials. Grover has clearly missed the part in Rule 122A that requires all new drug applications to be accompanied by “information and data as required by Appendix I or Appendix IA of Schedule Y, as the case may be.” Schedule Y lists all data that is to be submitted to the DCGI – in particular Clause 1(iv) of Schedule Y, identifies the following as relevant data: “…human clinical pharmacology data as prescribed in Items 5, 6 and 7 of Appendix I”. A reference to Items 5, 6 & 7 of Appendix I indicates that those items reference Phase I, Phase II & Phase III clinical trials as described in Schedule Y which can be accessed here. It is thus clear that data for Phase I, Phase II and Phase III clinical trials is required to be submitted to the DCGI.
I therefore do not understand how Grover is claiming that Rule 122A requires only “data” and not “Phase III clinical trials”.
Rule 122A and waiving of Phase III clinical trials abroad
This is the crux of the argument and involves the legal interpretation of Rule 122-A and its proviso. To appreciate the rival contentions it is important to reproduce both the main sub section (1) (2) and the proviso.
122-A
- (a) ….
(b) ….
Provided that any application received after one year of the grant of the approval and the sale of a new drug, shall be accompanied by … such information and data as required by Appendix 1 or Appendix 1 A of Schedule Y, as the case may be.
“(2) The importer of a new drug when applying for permission under sub rule (1), shall submit data as given in Appendix 1 to Schedule Y including the results of local clinical trials carried out in accordance with the guidelines specified in that Schedule and submit the report of such clinical trial in the format given in the Appendix II to the said Schedule;
Provided that the requirement of submitting the results of local clinical trials may not be necessary if the drug is of a cha nature that the Licensing Authority may, in public interest decide to grant such permission on the basis of data available from other countries.”
[Underlining is for convenience]
It is Mr. Reddy’s contention that as the main provision, that is, sub-rule 2 of Rule 122A, requires that when an application is made for import of a new drug the data required to be submitted is in accordance with Appendix 1 of Schedule Y (which includes phase III clinical trial data from other countries) the same applies for the proviso. This argument is flawed.
It is a settled rule of law of interpretation that where the meaning of a provision is plain, it should be given effect to.
When one reads rule (1), sub rule (2) and the proviso, it is clear that in sub rules (1) (2) the Legislature has consciously used the long-winded phrase “shall submit data as given in Appendix 1 to Schedule Y, whereas the proviso does not use that phrase or even the phrase, “the said data or information.” So, when the Legislature wanted the licensing authority to use the data as specified in Appendix 1 of Schedule Y, it said so. In the Proviso it consciously avoided that phrase. ”Instead, it used the expression – “data available from other countries.” The plain meaning of the two phrases is different. Thus, on a plain reading of both the expressions, it is clear that the data required for the invocation of the proviso is not the same data as stipulated in main provisions of sub rule (1) or (2). It is data from other countries, plain and simple and not restricted to data specified in Appendix 1 of Schedule Y.
Further quoting Mr. Reddy:
“It should be noted that the above proviso does not state “Phase III trials” may be waived – it only states that “local clinical trials” may be waived, which clearly means that the rule maker was expecting some kind of Phase III trials.”
Mr. Reddy does not seem to notice the ‘Notes’ to Appendix 1 of Schedule Y which state: “(1)All items may not be applicable to all drugs. For explanation, refer text of Schedule Y.”
It is unclear on what authority Mr. Reddy concludes that items 5, 6 and 7 of Appendix 1 (which pertain to clinical trials) are applicable to all drugs and at all times.

Tubercolosis bacteria. Credit: Public domain
In my article, I had referred to the text of Schedule Y, which states: “(3)For drugs indicated in life-threatening/serious diseases or diseases of special relevance to the Indian health scenario, the toxicological and clinical data requirements may be abbreviated, deferred or omitted, as deemed appropriate by the Licensing Authority.”
Mr. Reddy’s argument that submission of Phase III data is an absolute must is neither supported by the language nor the overall scheme of Rule 122A, Schedule Y and Appendix 1.
It is possible to argue that the meaning of the proviso to sub-rule (2) is not plain as I make it out to be and there is ambiguity. For that, the rule of purposive interpretation has to be followed. The purpose of the proviso, which can be gleaned from the expressions “drug of such a nature” which involves “public interest” is to cater for situations that cannot be foreseen, including health crises of a sudden nature, like the Zika or Nipah outbreaks or other larger and deadly epidemics like MDR TB.
There are two conditions to be satisfied.
Firstly, the drug has to be of a particular nature, which must involve public interest. Secondly, in respect of that drug, data must be available from other countries. Only upon the satisfaction of these conditions can the licensing authority decide to grant the approval. It is my contention that this provision should be invoked only in exceptional circumstances. The MDR TB scenario in India – with thousands of patients facing imminent death is one such exceptional circumstance.
The proviso doesn’t kick in on the arbitrary whims and fancies of the authority. It is to be exercised on the basis of objective conditions existing and the subjective satisfaction of the same by the authority. The provision is not amenable to an interpretation to allow “a blanket license” or a get out of jail free card expect more pharmaceutical companies to invoke the provision to seek complete waivers,” as Mr. Reddy wants to paint my argument.
It needs to be appreciated that even if the approval is granted it can do with strict rollout conditions, only in public hospitals etc. The approval/permission need not be a blanket one as Mr. Reddy makes it out to be.
Safety of bedaqualine
On the safety of Bedaqualine, Mr. Reddy and other critics have talked of increased QTc interval prolongation of the heart. This has been conflated “adverse reactions with the cardiac rhythm,” by others who support Mr. Reddy’s point of view, and therefore bedaqualine is deemed to be unsafe. Factually, this is not correct. But I am deliberately not getting into it.
The reason is that issue of drug safety is not matter to be resolved by lawyers, either by me, despite the fact that I am a qualified biochemist, or Mr. Reddy, or as a result of a debate between us. Neither of us are scientific experts to decide whether the data is sufficient to allow for restricted use. Admittedly, the WHO is an international authority and it has recommended the use of drug and later revised its assessment continuing the recommendation on account of better results. Mr. Reddy himself cites that the latest WHO assessment shows that 63% of the persons living with MDR TB were cured. It is for experts to take a call on that. And they have done it, in my opinion, in accordance with law.
In this context, Sub-Rule (3) of Rule 122A is relevant:
(3) The Licensing Authority, after being satisfied that the drug if permitted to be imported as raw material (bulk drug substance) or as finished formulation shall be effective and safe for use in the country, may issue import permission in Form 45 and /or Form 45A, subject to the condition stated therein;
Provided that the Licensing Authority shall, where the data provided or generated on the drug is inadequate, intimate the applicant in writing and the conditions, which shall be satisfied before permission, could be considered.”
Thus, a conditional approval is a possibility, contrary to Mr. Reddy’s claim.
It is my submission that the government has been lax in rolling out bedaqualine and that Mr. Reddy’s arguments are adding fuel to the fire. In contrast to India, South Africa has been very proactive in rolling out bedaquiline. The results coming out of South Africa at their fifth Annual TB Conference, Durban, shows a significant decreased mortality in persons who got bedaqualine compared with those who did not. This decreased mortality occurred even though people who got bedaquiline were sicker and had more resistance. The good news is that the government is scaling up the use of bedaquline.
The question is, if the use of bedaqualine is going to cure two out three persons, and in its absence, they would face certain death, would any reasonable medical person withhold that drug from those persons. That is question that the learned professor, Mr. Prashant Reddy, has been avoiding and would like to avoid, but needs to answer.