There is no clear line of treatment of PCOS/D and women are seen as ‘different’ or ‘unfeminine’.

Diagnosis and treatment, both are almost inaccessible for women who do not live in cities. Credit: Pixnio
As a woman of reproductive age with a regular menstrual cycle who has decided to not have children, I did not have a go-to gynaecologist. This was the case until one menstrual period when the cramps were so painful that I was forced to look up doctors. I went to one who came highly recommended on the gyaenacs you trust list.
She asked for an ultrasound as a routine check. It was then that we found multiple cysts on my ovaries. I stared at the ultrasound and looked up ‘normal size of ovaries’ on the internet. I found that mine were four times the normal size. A ten minute face-to-face with the doctor gave me the diagnosis – polycystic ovarian syndrome/disorder (PCOS/D).
PCOS is an endocrine disorder that affects women of reproductive age. Multiple cysts on the ovaries obstruct the regularity of the menstrual cycle and this could result in infertility. The condition presents itself in several other forms as well – increased facial hair growth or hirsutism, obesity, anxiety and depression.
However, there is no clear system for either the diagnosis or treatment of the disease yet as this story will establish with the help of inputs from women who suffer from PCOS. The symptoms range from hirsutism and obesity to mood swings, making it hard to pin it down. Ultrasound – to spot multiple ovarian cysts – helps detect PCOS only in 30% of cases.
The treatment is still centred around fertility treatment, isolating women who do not wish to conceive. And it ranges from advice to take contraceptive pills to diet to meditation.
Why I started an online survey on women with PCOS
In early 2017, a news report spoke of a woman college principal in India who told her students that dressing like a man/boy causes PCOS in women. It highlighted how symptoms of PCOS are regarded in society, positing the patient as ‘being like a man’ or being ‘less of a woman’.
As someone with PCOS, I have struggled with accepting the symptoms and problems of the condition. I have changed doctors several times in the hope that I will be prescribed a solution above and beyond the immediate reproductive concerns. I was told, as are most women with PCOS, to take an oral contraceptive till I am ready to conceive.
‘It will go away if one gets married and has kids’ or worse, ‘it is a part of life’ are the other common gynaec responses to the condition.
As I struggled with the many issues that hitchhiked on this diagnosis, I decided to conduct a short online survey to understand and document the experiences of women with PCOS. I was surprised at how quickly and willingly 81 responses poured in within two weeks.
A lot of the responses showed how women dealt with the condition as well as the hurtful reactions of a society that seemed to uphold a standardized view of femininity. Many women felt isolated because of the lack of accurate information and understanding about PCOS.
Here are some outcomes and insights of this short survey.
‘I spent 15-20 years not knowing what the problem was’
The survey found that 32.1% of the women who were diagnosed were between 21-25 years; 30.9% were older. It is possible that more than half the diagnoses were recent because there is now increased awareness about the condition among both doctors and women.
Those diagnosed as early as 12-15 years of age, 14.8% respondents, reported some of the most difficult experiences. “When I was diagnosed there was no Internet and for the first 15-20 years there was a sense of not knowing how to find out more,” said Sneha*. “There was a sense that if I did not want to marry or have children, there wasn’t really a big urgency around my issues.”
We know that the most common reason women go to a gynaecologist is an inability to conceive and/or irregular periods. These are considered classic symptoms of PCOS. Diagnostic techniques varied – from ultrasounds to an endocrinologist hazarding a guess that the problem could be PCOS. Many were recommended tests or scans because of the presence of facial acne, heavy bleeding and excessive facial hair.
The problem of diagnosis: symptoms could be typical or unusual
The criteria for diagnosis is spread across three areas – cosmetic (hair growth, hair loss), reproductive (irregular periods, painful periods, cysts on ovaries) and hormonal (increase in testosterone levels, problems with insulin – resulting in weight gain, depression and anxiety because of hormonal imbalance).
The extent to which women suffered these symptoms varied. Even multiple ovarian cysts are not always present in women diagnosed with PCOS but they complained of irregular periods or suffered hormonal imbalance (prolactin, testosterone, thyroid and so on) which led the doctors to treat it as PCOS.
Patients who have more than a few symptoms – irregular periods, weight gain, hirsutism, hormonal imbalance, hair loss, anxiety and depression – are diagnosed with PCOS. Several women who had regular periods were diagnosed with PCOS after the ultrasound revealed cysts.
This is important to understand because it is likely that many women who have PCOS are not getting any treatment because they have not been diagnosed or suffer unusual symptoms.
Women feel isolated, ashamed they aren’t ‘feminine’ enough
While researching the condition, I did several searches on the Internet. Several links that showed women’s frustration with the system of diagnosis. There is shame attached to the condition and women seemed to fear isolation and contempt they would suffer because they are ‘different’.
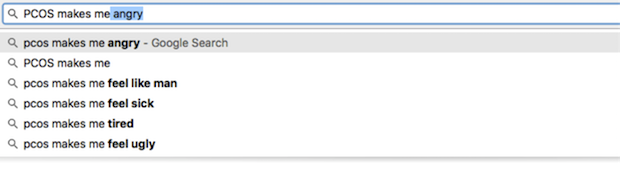
A quick search of ‘PCOS makes me’ – prompted the following answers:
Some of these responses showed up in the survey as well. Self-esteem took the worst hit. It is thus common to hear statements about ‘unfeminine body’.
More than 25 women surveyed discussed issues related to appearance – increased facial hair, loss of hair on the head. Some women reported being uncomfortable about their condition and others said they were bullied in school.
“Dealing with the hirsutism was very embarrassing. It made me self-conscious to the extent that intimacy makes me anxious. Hirsutism is also hard to tackle/eliminate, because cosmetic solutions are frightfully expensive,” said Sarita*.
Smita* was bullied in school because of her facial fair which led to self-esteem issues. She even tried laser treatment. When it didn’t work, she got into the habit of shaving the excessive hair on her cheek and jaw. She added that she sometimes resists her impulses by letting her body hair grow out now for months together.
“I still shave every other day. I dream of eventually working up the courage to let my facial hair grow out fully and wearing shorts with my leg hair showing. I hate that I believe that one’s hair should not affect one’s self-perception but this, the contrary, too is still deeply ingrained in me,” said Smita*.
Another woman spoke of prolonged periods and exhaustion as one of her concerns. The fact that she ‘has scars from years of acne on her face is a problem she cannot fix’ is equally troubling for her.
No medical help if you live in villages or small towns
Diagnosis and treatment, both are almost inaccessible for women who do not live in cities. A respondent from Assam wrote about her expensive and tiresome journey to Kolkata to figure out her condition. She had irregular periods for many years but did not visit a doctor till she started suffering severe pain in the pelvic region.
“On one visit to Calcutta I found that I had PCOS and was given medicines for it. Much later, an ultrasound revealed that I no longer had PCOS,” she said. “However, my prolactin was high which, the doctor said, caused the anxiety issues I’ve had for a long time. The prescribed pills eased the pain but my periods stayed irregular. The gynaec recently asked me to take more pills and be patient with the treatment.”
Several women diagnosed with PCOS said doctors were not responsive and did not mention issues like insulin resistance if they weren’t ‘fat’. For others, even ‘huge lifestyle changes (eating better, exercising and sleeping better)’ did not help stabilize the menstrual cycle.
Fertility is still the main focus of treatment
Several women contest the treatment of PCOS because the focus is primarily on fertility and weight loss. But there are many other problems related to PCOS. For instance, there is now research being done on how it is directly related to thyroid conditions.
There is also a lot of debate about the side effects of the oral contraceptive pills that are routinely prescribed for PCOS. These include increased risk of depression and anxiety. The doctor did not mention these side effect to me while prescribing them. However, we did switch from one oral contraceptive to another because one of them led to severe headaches, similar to migraines. She said this was common because not all oral contraceptive pills suit all women.
Women who’ve taken the survey concur that they suffered mood shifts (more anxiety) even as their periods stabilized along with regularity of their periods. The regular periods urged several of them to stay on the pill.
The survey found that some doctors (23.5%) recommended several options including the pill, inositol and metformin for insulin resistance and exercise. And 22.2% recommended only the pill.
More than half (60.5%) the women felt they were excluded from decision making when it came to treatment. Several turned to alternate medicine because they did not get enough information from their doctors. Many chose to simply diet and exercise.
Doctors do not share information or discuss treatment
I got answers to my questions about PCOS from the internet and other women with PCOS. The survey showed that 29.5% of the women felt that they were not getting enough information about their own body.
Of those who were informed, 71.6% had got their information from doctors. However, not all women were given the same information by their doctors.
There was a huge difference in what they were told about insulin resistance, fertility, cramps, anxiety and depression. Some were brushed off with only one answer: “Infertile.”
Raji* was 12 when she was diagnosed with PCOS. She was told about hyperinsulinemia – having excessive insulin in one’s blood – being the root cause of PCOS which is currently being assumed as one of the main causes and asked to keep a tab on her weight. “I was even asked to meditate to help my body. But as a 12-year-old I did not understand the magnitude of these suggestions. I was more concerned about the hair growth and the cosmetic solutions for them.”
Raji got correct, if overwhelming, information. But some were given ‘vague suggestions about weight loss’ or told it would be ‘a lifelong problem’. Some doctors even scared women into losing weight by showing them ‘a diagram of a woman with heavy hair growth on the stomach and chest’.
Looking for a good doctor: why it is tough with PCOS
Dissatisfaction with a particular doctor’s approach or relocation led many women to new doctors. Some women were given different versions each time: “First doctor said I’d have problems conceiving. At 15, that was the best news ever. The second doctor told me about susceptibility to heart diseases and diabetes, which scared me more,” said a respondent.
Since weight gain is a huge concern for women several doctors discussed losing weight. However, the experiences of women show that this was difficult.
Samia* said that after her visit to the doctor she became an ‘exercise addict’. “My family and friends used to make jokes about it initially, which made life difficult, what with already being depressed about having PCOS. Now, after four full marathons, they’re proud of me,” she said.
One of the respondents found the diet, exercise, sleep, medicine routine tiresome and stressful. “God forbid you have a depressive episode and fall off this carefully constructed wagon. You are back at the beginning. Hormones are unforgiving that way,” she said.
Flagging libido and why few talk about it
There is agreement in the survey that doctors need to dedicate more time to finding a patient specific treatment plan. Women’s experiences and a few studies indicate that not enough has been done to understand the link between PCOS and fall in female libido.
This could be the psychological effect of being overweight or battling hair growth. (Many women in these studies said that PCOS made them feel less attractive to their partners and sometimes even less feminine.) Depression and anxiety caused by hormonal imbalance could be another reason.
In studies conducted on women with PCOS, it is seen that they are significantly less satisfied with their sexual lives than women who do not deal with the syndrome.
“We need more access to PCOS-specific diet plans. Doctors need to address daily life problems such as acne, libido, hair growth. These things matter. Most docs just keep telling me to have a kid soon,” said Shreya*.
Trans men can suffer too
Currently, the focus in research being undertaken globally on PCOS are related to diagnostic techniques and treatment. The focus is entirely on the cisgender heterosexual (cis-het) women i.e. those who are heterosexual and identify with the gender assigned at birth.
In my own study, most of the responses were from women who identified as female. However, researcher Shruti Rao who did her Masters dissertation from British Columbia University on PCOS, found in her own research that PCOS assumes a cis-het female patient which makes trans-men an invisible community in terms of patient support and outreach.
“Of the very little and sporadic research done on sexuality and sexual identity with respect to PCOS, there are indications that over 50% trans men (in that small study) could have PCOS,” she said.
Turning to each other or support
As science still struggles to find answers, many women have turned to online platforms both for support as well as information. Facebook groups, nutrition e-mailers for a PCOS diet and a multitude of online forums are filled with women sharing their experiences and offering/finding support.
71.6% of the respondents stated that the condition should have a support system because of the isolation the syndrome brings.
Several women find themselves pressured to have children but have to go through a lot of changes in their lives without any emotional support from family or peers.
“As someone who was not diagnosed and suffered for more than 15 years, I always sought women who were in my experience basket,” said Radha*. “You need a support system to encourage you stick to the modified lifestyle, exercise regimen, diet chart. You also need someone to push you to schedule regular doctor appointments.”
Some online groups/forums do extend different kinds of support to women. Soul Cysters is among the most popular. However, my experience shows that the forums offer support mostly to women who are finding it difficult to conceive though they have sections dedicated to depression, anxiety and so on.
“While it is safe space for women to be present, it can leave the rest of us who don’t want to have children silenced and fending for ourselves in terms of treatment/management,” said Raksha*.
Way forward: PCOS means multiple issues, deal with them
For many women, the condition goes beyond reproductive issues as discussed earlier. It is believed to affect not just one’s moods, libido and fertility but also increase susceptibility to diabetes, cardiac problems and possibly even cancer.
“A lot of my trauma has been mental. I feel I am missing out on a very basic bodily rhythm – I envy women who know when their next menstrual cycle begins,” said a respondent.
While several women said they found it difficult to handle the physical, psychological and social issues associated with PCOS, others said they were able to ‘take back control and kick start a journey of healing’ and ‘appreciate the body with a renewed perspective’.
Treating people with multiple health issues is always complex, researchers have said. It’s also hard for such patients to find a suitable doctor, an effective line of treatment and feel like whole beings.
“Zero surprise that the two biggest focuses of the condition – medically and socially – seem to be subsumed into the infertility and weight-loss industries which are huge cash cows for the medical-industrial-complex,” said researcher Shruti Rao. Hirsutism adds to this, she pointed out.
However, it would make all the difference to ‘tackle obesity, hirsutism and possible infertility as functions of a syndrome/condition rather than as moral judgements’, said Rao.
It is thus important for the medical community to address the varied experiences of women and trans-men in their work and research. The hope is that more conversation among women, researchers and doctors would lead to the patient being included in the decisions made about their body. And greater awareness of a patient as an individual, not just a reproductive being.
Note:Names have been changed to protect identity.
Srinidhi Raghavan is a freelance writer.
This article was originally published on IndiaSpend. Read the original article.